This study examines the impact of this transition on medical students at a public university by focusing on their academic performance, emotional well-being, and adaptability to remote learning environments. Since the COVID-19 pandemic prompted an unprecedented shift from traditional classroom learning to online platforms across global educational systems, it is crucial to understand how students navigated these changes and adapted to the new learning conditions. This study collected qualitative data from 65 medical students through semi-structured interviews. The findings reveal significant effects on study habits, emotional well-being, and curriculum engagement. The findings reveal a mixed response to distance education in medical schools. While some students experienced increased flexibility and, in some instances, improved academic performance, significant challenges also emerged. These challenges included a decline in practical skills, heightened emotional distress, and technical issues that obstruct effective learning. The study emphasizes the necessity for hybrid educational models that combine the advantages of online flexibility with essential in-person interactions, particularly for training practical skills in medical education. It recommends enhancing online educational platforms to better support medical training during crises. Emphasis is placed on developing a robust technical infrastructure alongside comprehensive mental health support systems.
____________________
Journal of Digital Pedagogy – ISSN 3008 – 2021
2025, Vol. 4, No. 1, pp. 36-48
https://doi.org/10.61071/JDP.2524
HTML | PDF
____________________
Introduction
Technological advancements and innovations influence all social life and institutions, including higher education. As the number of medical students in higher education continues to grow, new approaches have emerged to address the information needs of the 21st century. In this context, new behaviors and roles for academicians have emerged in response to the unique demands of distance education, which is becoming increasingly essential in 21st-century university settings. Distance education has transitioned educational materials into interactive virtual environments, making learning more accessible and adaptable. Technological advancements have enhanced the practicality and cost-effectiveness of distance education in higher education. Specifically, the economic benefits of efficiently allocating limited resources across different geographic locations and time zones have expanded the reach of distance education, creating a broader market for remote learners (Totaro et al., 2005; Moore & Kearsley, 2012). As Clark (2022) noted, distance education has a rich history spanning nearly 300 years, beginning in the 1700s when Caleb Phillips from Boston offered shorthand lessons via weekly mail. The first instance of electronic distance learning emerged in the 1920s, with courses broadcast over the radio. The rise of the internet has since initiated a significant transformation in distance education, enabling a wide range of educational institutions, associations, and organizations to provide remote courses, especially in healthcare technology. Distance or online learning is not a novel concept; however, it signifies a substantial transformation from traditional classroom models, particularly for academic medical professionals (Kentnor, 2015). Additionally, it delineated essential strategies for developing effective online learning platforms within the medical field, highlighting the necessity of user-friendly and intuitive website design and incorporating self-assessment tools to enhance learner engagement (Schneider & Council, 2021).
Dron (2021) has extensively explored the concepts of distance education and educational technology. His work emphasizes that teaching is fundamentally a technological process involving various forms of “distance” between learners and teachers. These distances can be physical, temporal, structural, social, emotional, cognitive, cultural, pedagogical, or technological. He suggests that understanding these multiple dimensions is crucial for effective distance learning. Since the early 1980s, distance education has undergone remarkable growth on both national and international scales. It has transitioned from early correspondence education primarily relying on print-based materials into a global movement leveraging various technologies. As an alternative to conventional education, distance education provides degree-granting programs, addresses illiteracy in developing nations, offers training opportunities for economic advancement, and enriches curricula in non-traditional educational contexts. The potential of distance education is extensive, presenting solutions to numerous educational challenges and promising a progressive future for medical education. Various technologies have been employed as delivery systems to facilitate this learning mode (Gunawardena & McIsaac, 2013).
The global COVID-19 pandemic has profoundly disrupted traditional education, leading universities worldwide to suspend in-person classes to curb the spread of the virus. In response, many medical schools transitioned to online learning, where instructors and students are often separated by distance and time, fundamentally altering how medical knowledge is imparted and absorbed. In December 2019, the emergence of a new virus outbreak known as COVID-19 in Wuhan, China, rapidly escalated into a global pandemic, significantly impacting numerous nations (World Health Organization [WHO], 2020). The WHO formally declared this outbreak an international public health emergency on January 30, 2020 (WHO, 2020). The swift transmission of the virus has compelled many countries to implement stringent measures to curb its spread. Various organizations have experienced profound disruptions due to the pandemic, and the closure of educational institutions has adversely affected children, young adults, and adults alike (UNESCO, 2020). Hughes et al. (2020) assert that the COVID-19 pandemic has posed considerable challenges across all dimensions of healthcare. The imposition of lockdown measures and the necessity for social distancing have markedly diminished teaching opportunities for trainees, severely restricting their hands-on learning experiences and exposure to authentic clinical environments.
Coman et al. (2020) emphasized that the global COVID-19 pandemic has profoundly affected higher education’s teaching and learning processes, particularly regarding teacher-student interactions. Consequently, educational institutions were necessitated to transition all activities online. This shift, which effectively relocated classrooms to students’ homes, may have transformed students’ perceptions and experiences of online instruction. Furthermore, the pandemic prompted universities worldwide to suspend in-person learning to mitigate the spread of the virus. Specifically, medical schools implemented various policies to cease face-to-face education. Many institutions suspended clinical rotations and reduced hospital exposure hours for undergraduate and postgraduate students. This reduction in practical experience has raised significant concerns among medical students, residents, and fellows (Siddiqui, 2020).
The rise and widespread adoption of distance learning systems has necessitated a critical evaluation of the strengths and weaknesses of various programs. In response, many new initiatives have been developed to address the growing demands of higher education, promote flexible learning environments, and support lifelong learning (Gunawardena & McIsaac, 2013). Tran (2016) noted that students utilize Learning Management Systems (LMS) such as Blackboard, Desire2Learn, Moodle, and Canvas, among other platforms, to access online learning environments. These systems typically facilitate asynchronous learning, allowing students to engage with course materials and complete assignments at their own pace, from any location, and at times that work best for their schedules. This level of flexibility empowers learners to tailor their educational experience to their individual needs and availability.
Medical schools worldwide adopted various policies to suspend in-person education during the pandemic. Many institutions halted clinical rotations and reduced hospital exposure for undergraduate and postgraduate students. This substantial decline in hands-on experience and procedural training has raised serious concerns among medical students, residents, and fellows about the potential impact on their education and clinical proficiency (Ahmady, 2021). In medical faculties, information technology tools are generally user-friendly and straightforward to operate, which has proven to be a crucial advantage in addressing the challenges brought by COVID-19, allowing educators to continue providing instruction to students. The pandemic has transformed traditional classroom interactions into a model that emphasizes individualized instruction for asynchronous learning, enabling students to access educational material anytime and anywhere without limitations (Daroedono et al., 2020).
This study seeks to investigate the actual perceptions of medical school students regarding distance education, a topic of growing significance as the world transitions to remote learning alternatives. Gaining insight into the viewpoints of these students is essential for assessing the effectiveness and potential drawbacks of distance education in the medical field. Furthermore, the perspectives of medical professionals can provide valuable information about the advantages and challenges associated with distance learning in this sector. Consequently, this paper aims to address the following questions:
RQ1. What changes did the remote education process during the COVID-19 pandemic bring to your habits compared to in-person education?
RQ2. How did you feel when the pandemic began, and your university suspended in-person classes? What emotions and thoughts were you experiencing at that time?
RQ3. What challenges did you encounter during the initial and ongoing phases of the academic term? Did you effectively communicate these concerns to your instructors?
RQ4. What are the advantages and disadvantages of remote instruction in medical education?
RQ5. How did remote education impact your overall grades?
Medical Education within the Higher Education System
Turkey’s medical education system is designed to provide comprehensive training for future healthcare professionals by integrating theoretical knowledge with extensive clinical practice. Regulated by the Council of Higher Education (YÖK), the system follows a six-year undergraduate program, where students acquire a strong foundation in basic medical sciences before progressing to clinical rotations and concluding with a one-year hospital internship. Public medical education programs adhere to this structure, with the final three years primarily focused on clinical training (YÖK, 2020). Students engage in theoretical lectures, seminars, and hospital rotations during this phase, ensuring a well-rounded and practical learning experience. However, before the COVID-19 pandemic, medical schools in Turkey had not widely adopted distance e-learning as an instructional approach, relying instead on traditional in-person training. Although the pandemic necessitated a sudden shift to online education, integrating digital learning into medical training remains a challenge, given the essential role of hands-on experience in developing clinical skills. Following the national lockdown, medical students were compelled to swiftly transition to distance learning at home, with minimal preparation time. Both faculty members and students confronted unprecedented challenges and had to develop their skills to sustain the educational process rapidly (Başer et al., 2020). The pandemic was extremely challenging for pre-graduation medical education, requiring rapid and sometimes instant decision-making beyond the defined processes in an uncertain environment in Turkey. In this context, the pandemic period highlighted the need to strengthen existing decision-making mechanisms, increase awareness of the importance of quality cycles in medical education, and create opportunities to accelerate work in certain areas (Akan et al., 2021). For instance, infrastructure studies of committees and commissions, such as assessment and evaluation, curriculum, and program evaluation—whose preliminary work had already begun—were expedited and completed.
2. Methodology
2.1. Research Design
This study employs a qualitative research method rooted in a phenomenological design. This approach revolves around phenomena we may be familiar with but lack a comprehensive understanding. Phenomenological studies aim to explore individuals’ experiences, perceptions, and the meanings they assign to a phenomenon (Yildirim & Simsek, 2018). This research investigates students’ perspectives from the public university faculty of medicine regarding the distance education process in higher education in the aftermath of the COVID-19 pandemic, along with their insights into the challenges faced and suggested solutions.
2.2. Study Group
This study used convenience sampling, a purposeful sampling method that enhances the relevance of the information gathered from a smaller sample in relation to the research objectives. The participants were selected based on their ability to provide valuable insights into the phenomenon being explored (Patton, 2014). Convenience sampling offers advantages in terms of speed and ease, as it allows researchers to select participants who are nearby and easily accessible (Yildirim & Simsek, 2018). The study included 65 medical students, all of whom volunteered to participate—43 male and 22 female medical school students. These students were chosen for their experiences with remote education. Specifically, students from the 1st, 2nd, and 3rd years were selected, as they extensively use digital tools.
2.3. Data Collection and Analysis
This study employed semi-structured interviews to gather insights from medical students. The collected data were analyzed using content analysis, a qualitative research method. To ensure the clarity and relevance of the interview questions, the researchers consulted two experts in educational management (Patton, 2014), and the questions were further reviewed by specialists in medical education, leading to the final version of the interview format.
MAXQDA 24, a qualitative data analysis software, was used for data analysis and a descriptive analysis approach. Themes and sub-themes were identified from participants’ responses, and frequency counts were used to determine how often each theme appeared. Direct quotations were included to reflect participants’ perspectives. Each participant was assigned a unique code (P1–P65) to ensure anonymity in the reporting process.
The semi-structured interviews followed a structured protocol:
- Introductory Phase – General questions to establish rapport.
- Experience Sharing – Open-ended questions about participants’ experiences with distance education.
- Focused Questions – In-depth exploration of challenges and adaptations encountered.
The interview questions were pilot-tested with a small group of students to refine clarity and relevance, and each interview lasted approximately 45 to 60 minutes.
2.4. Validity and Reliability
Multiple data sources were incorporated to strengthen the validity of the findings. Academic performance data such as GPAs before and during the transition to online education were analyzed to establish potential correlations between students’ experiences and their academic outcomes. Metrics regarding students’ online participation (e.g., attendance in virtual classes, completion rates for assignments) were collected to provide an objective measure of engagement and correlate with qualitative findings.
2.5. Methodological Limitations
The study has limitations. The use of convenience sampling may lead to a bias, as the sample may not fully represent the broader medical student population in Turkey, given that those who volunteered may have had more favourable views of distance education. Findings from a single medical school may not be generalizable to other institutions with different curricula and distance education approaches. The subjective nature of qualitative research means that respondents’ interpretations of their experiences can vary significantly, potentially affecting the conclusions drawn from the data.
3. Findings
This section outlines the context and objectives of studying medical students’ experiences while transitioning to distance education. Based on participants’ experiences, the findings are categorized into primary themes and sub-themes.
RQ1. As regards the first research question, “What changes did the remote education process during the COVID-19 pandemic cause in your habits compared to face-to-face education?” the participants offered the following insights:
Figure 1
Themes 1: Changes in Habits Due to Remote Education During COVID-19
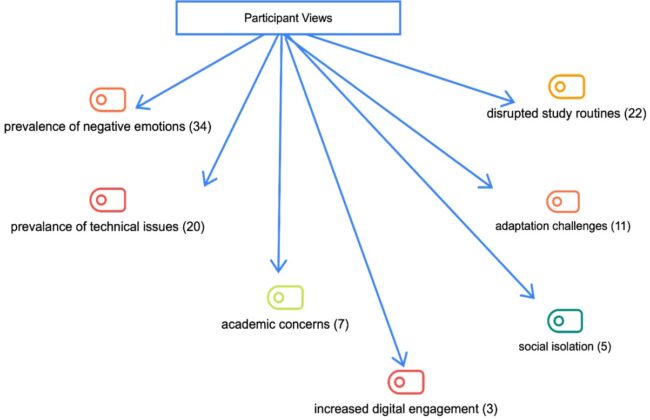
This first diagram illustrates the key themes identified from participants’ responses regarding changes in habits due to remote education during the COVID-19 pandemic. The most prominent theme is the prevalence of negative emotions, with 34 participants indicating that emotional strain was a significant challenge for many during this period. Disrupted study routines (N:22) and technical issues (N:20) were also commonly reported, underscoring the practical difficulties students encountered while adapting to the online learning environment. Further, adaptation challenges (N:11) and academic concerns (N:7) suggest that the transition to remote learning posed considerable obstacles in adjusting to new educational methods and maintaining academic performance. On a social level, the theme of social isolation (N:5) reflects the loss of interaction and engagement typically found in face-to-face education. Notably, only a few participants (N:3) reported increased digital engagement, indicating that while some students embraced the digital transition, this was not the prevailing experience. In summary, the analysis reveals remote education’s negative impact on students’ emotional and academic habits, with technological and structural challenges playing key roles.
Some participants expressed their views as follows:
I used the internet actively and became more individualized P65. I disrupted my study routine, started listening to lectures less, and spent the time I used to prepare for class sleeping P45.
There was no change; my sleep pattern was disrupted, and my eating hours and routines changed P60. It was very productive, and I realized face-to-face education was ineffective P50.
My study routine was disrupted; I used more technological devices, woke up later, and felt more comfortable, but my study time decreased P12. I got used to studying online, experienced increased computer usage, studied in a relaxed environment at home, felt lethargic, and became more relaxed and undisciplined P6. I found more time to study, but my sleep pattern was disrupted, and my motivation decreased P1. Laziness increased, I moved less, and I felt good in a comfortable environment P23.
RQ2. In addressing the second research question, “How did you feel when the pandemic began and your university suspended in-person classes?” the participants shared a variety of thoughtful and insightful responses, which are detailed below:
Figure 2
Theme 2: Emotional Responses to the Suspension of In-Person Classes
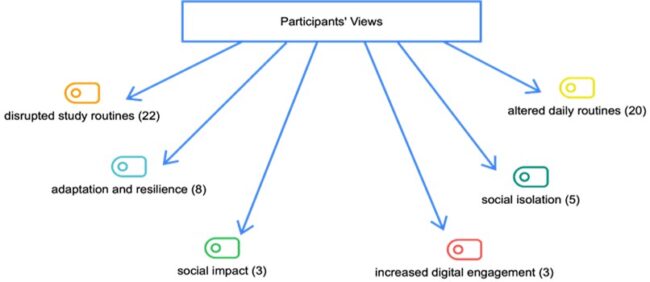
The diagram outlines several key themes derived from participants’ perspectives on the changes brought about by remote education during the COVID-19 pandemic. Notable concerns include disrupted study routines (N:22) and altered daily routines (N:20), indicating that the transition to online learning significantly affected academic and personal schedules. The theme of adaptation and resilience (N:8) highlights that, despite the challenges, some participants exhibited flexibility and strength in adjusting to the new learning environment. Conversely, social isolation (N:5) and social impact (N:3) underscore the negative effects of reduced social interaction during remote education. While only a small percentage of participants reported increased digital engagement (N:3), this suggests that a few individuals took advantage of remote education opportunities to utilize digital tools better. Overall, the analysis reveals a balance between challenges and coping strategies. Many participants struggle with disrupted routines and social isolation, while some demonstrate resilience and adaptability in navigating the digital learning landscape. This emphasizes the need for structured support to reduce disruptions and enhance social and academic experiences in distance education.
Some participants expressed their views as follows:
At first, I was happy, but as the process continued, problems arose (P3). It was an unwanted situation; boredom, concerns about the future, and uncertainty made me despair (P5). I was very sad (P6), I was very upset (P7), but then I became happy (P9).
Laboratory classes were disrupted, we could not socialize, and we became withdrawn. At first, it felt like a vacation, but then I experienced unhappiness P32. I wondered if I would ever go back to university again. I was very sad, and I felt terrible, P36. I was worried that people who did not deserve it passed their classes, and I felt sad because I felt sad, our social interactions were limited to P29. The classes were ineffective, and I felt uncomfortable because my routine had changed to P3.
RQ3. To address the third research question, “What issues did you encounter when classes commenced and continued? Did you communicate these challenges to your instructors as students?” The participants provided the following insights.
Figure 3
Theme 3: Challenges Encountered and Correspondence with Instructors
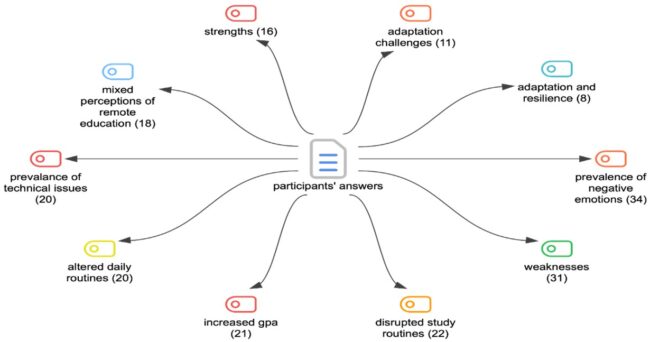
The third figure outlines the key themes from participants’ responses regarding their emotions and experiences during the pandemic and the transition to remote education. The most prominent theme identified is the prevalence of negative emotions, documented 34 times, indicating that emotional challenges were widespread as students adapted to this new educational landscape. Closely following this is the theme of perceived weaknesses, mentioned (N:31) times, which reflects the sentiment that many participants felt their academic performance or personal capabilities had been adversely affected. Despite these challenges, positive outcomes were also reported, with (N:21) stating that students experienced increased GPAs, suggesting that some individuals achieved academic improvement amid the difficulties. Everyday struggles included disrupted study routines (N:22) and altered daily routines (N:20), showcasing the significant lifestyle changes brought about by the pandemic. Additionally, technical issues were highlighted (N:20) times, underscoring the practical difficulties that compounded the stress of remote learning. Conversely, participants demonstrated strengths (N:16) and a capacity for adaptation and resilience (N:8), indicating their ability to cope and adjust over time. The theme of mixed perceptions of remote education emerged (N:18) times, revealing that while many faced challenges, some students acknowledged advantages or maintained a more balanced perspective on the new learning environment. In summary, the analysis indicates that while remote education during the pandemic posed numerous emotional and practical challenges, a segment of students managed to adapt and even excel academically, highlighting the varied impacts of this unique experience.
Some participants expressed their views as follows:
Medical education should never be online (P36). There cannot be distance education in medical education (P65). It is good to be able to repeat the same class (P48). There is no strength; its comfort and convenience reduce practical skills. The positive side is that it is easy to access all classes with a single click (P3).
We reached classes quickly, but it was inefficient; having online skills and laboratory classes was inefficient(P62). The opportunity to listen to classes again is a strength (P55). It becomes inefficient when there are internet issues; it can only be online for theory classes. We missed out on practical classes; the only strength of theory classes was the opportunity to listen again (31)
The class recordings were a strength, but the lack of interactive participation was a weakness (P43). Apart from the class recordings, the lack of practical classes was weak (P17). Distance education has no strengths, and the lack of practical education has no strengths. It is healthier for students to learn on their own. Only being able to listen to classes again is a strength, but it negatively affects practical classes (P30).
RQ4. The fourth research question analyzes the strengths and weaknesses of remote teaching in medical education.
The data presents students’ perceptions regarding the strengths and weaknesses of online education, particularly in medical education. The responses indicate a strong consensus on the limitations of online medical education, alongside a few acknowledged benefits.
Table 1
Themes 4: The Strengths and Weakness
| Subthemes | Codes | N |
| Strengths | Recorded Lectures | 65 |
| Ease of Access | 60 | |
| Flexibility and Convenience | 30 | |
| Weaknesses | Practical and Laboratory Learning | 65 |
| Lack of Interaction | 55 | |
| Reduced Skill Development | 50 | |
| General Inefficiency | 50 |
As seen in Table 1, many students appreciated the opportunity to re-watch recorded lectures, which greatly aided their understanding of theoretical concepts (N:65). The ease of access to lectures and course materials with a single click was also highlighted as a key benefit (N:55). Additionally, some students found the flexibility and comfort of attending classes from home advantageous. However, this sentiment was not universally shared (N:35). On the downside, the most significant concern was the challenge of replicating practical and laboratory learning online, particularly in medical education, which heavily relies on hands-on practice (N:65). Furthermore, many students reported a lack of interaction during online classes, limiting their ability to engage in discussions or ask questions—crucial components of deeper learning in medical education (N48). Reduced skill development was another critical issue, as students felt online learning fell short in providing the necessary clinical and practical experience (N:55). Technical issues, such as frequent internet connectivity problems, also disrupted the learning process, further diminishing the effectiveness of online education (N:55). Lastly, many students viewed online medical education as generally inefficient, with some expressing that it offered no significant advantages. At the same time, the absence of structure and discipline contributed to a perceived inadequacy (N:45).
Some participants expressed their views as follows:
Medical education should never be online (P36). There cannot be distance education in medical education (P65). It is good to be able to repeat the same class (P48). There is no strength; its comfort and convenience reduce practical skills. The positive side is that it is easy to access all classes with a single click (P3).
We reached classes quickly, but it was inefficient; having online skills and laboratory classes was inefficient(P62). The opportunity to listen to classes again is a strength (P55). It becomes inefficient when there are internet issues; it can only be online for theory classes. We missed out on practical classes; the only strength of theory classes was the opportunity to listen again (31).
The class recordings were a strength, but the lack of interactive participation was a weakness (P43). Apart from the class recordings, the lack of practical classes was weak (P17). Distance education has no strengths, and the lack of practical education has no strengths. It is healthier for students to learn on their own. Only being able to listen to classes again is a strength, but it negatively affects practical classes (P30).
RQ5. For the fifth question, did remote education affect your average grades? The participants provided the following explanations.
Themes 5. The Impact of Distance Education on Grade Point Averages (GPAs)
Table 2
Themes 5: The Impact of Distance Education on Grade
| Subthemes | Codes | N |
| Positive Impact on GPA | 55 | |
| Impact of Distance Education | Stable GPA | 20 |
| Negative Impact on GPA | 10 |
As seen in Table 2, the data provides valuable insights into how online education during the pandemic influenced students’ academic performance, particularly their GPAs. Most students (N:55) reported an increased GPA among the responses collected. This indicates that the transition to online learning offered many a more flexible and supportive environment, enabling them to manage their time more effectively, eliminate commute times, and access self-paced learning resources. In contrast, (N:20) participants noted no change in their GPA, suggesting that their academic performance remained stable despite the shift to remote instruction. These students may have adapted well, maintaining strong study habits and routines that translated successfully into the online format. However, another group of (N:10) participants experienced a decreased GPA, revealing some students’ difficulties with the new learning model. Issues such as a lack of motivation, technical difficulties, and limited interaction with instructors may have contributed to their decline in academic performance. In conclusion, while online education positively impacted the GPAs of many students, some faced significant challenges that resulted in either no improvement or a decrease in their academic performance. This variation in outcomes highlights differing levels of adaptability among students and underscores the necessity for more customized support during transitions to online learning.
Some participants expressed their views as follows:
My GPA increased, P3. My learning quality decreased. P7. I saw an artificial increase, P8, but there was no change. P9, my exams went well, and my grades increased. My grades increased because I listened to the revisions P18.
My grade increased, but that does not mean I learned P21. My GPA stayed the same, and not much change happened P56.
4. Discussion
The findings of this study reveal a complex and varied response to the shift to remote education during the COVID-19 pandemic, highlighting both the challenges and benefits experienced by medical students. Zhong (2020) highlights several critical factors that influence the effectiveness of online learning. Online learning may not adequately support students with kinesthetic learning styles and often fails to provide the social interaction commonly found in traditional classroom settings. These factors include limited access to resources, the availability of Internet connectivity, and students’ capacity to engage in digital learning environments. Furthermore, meaningful interaction with instructors is vital.
Modern medical schools are evolving from traditional, lecture-based pedagogies that rely on large classes and face-to-face instruction to a more student-centred approach. With the integration of IT tools, medical education has become increasingly personalized, fostering small team-facilitated discussions. This transformation encourages medical students to engage in self-directed learning, promoting individualized and interprofessional education (Daroedono et al., 2020). Furthermore, Asma and Tezci (2023) highlighted that distance education is particularly beneficial for disciplines such as the social sciences, where theoretical content can be effectively conveyed and where large classroom sizes often present logistical challenges for in-person instruction. They observed that the flexibility and accessibility of online learning can enhance educational outcomes in these areas, especially in the post-pandemic context. However, they also pointed out the potential drawbacks of applying distance education to subjects like mathematics, sciences, and engineering, where hands-on, practical learning is essential. Reliance on virtual platforms may create disparities in these disciplines, as students may not have equal access to vital resources or experiential learning opportunities.
In line with the findings, Sindiani et al. (2020) emphasized that limited social contact, including social distancing and the ability to save time and resources by not commuting to university, were among the most notable advantages of online learning. Additionally, a more streamlined learning process was identified as another significant benefit. However, the disadvantages included the necessity for sufficient technical setup, lack of face-to-face interaction, and restricted access to clinical environments. Furthermore, distance e-learning has the potential to serve as an effective alternative to traditional methods for delivering high-quality medical education. Nevertheless, integrating distance learning encounters substantial challenges, particularly in ensuring the availability of essential infrastructure and formulating effective institutional strategies (Panahi & Borna, 2014).
The findings from this study provide valuable insights into the experiences of medical faculty students during the transition to remote education due to the COVID-19 pandemic. While remote learning presented some advantages, such as increased flexibility and improved GPAs for many students, the challenges proved more substantial, especially in medical education, where hands-on training and practical experience are vital.
A significant theme that emerged was the disruption of students’ study routines and daily lives. Many participants noted decreased motivation and focus, difficulties adhering to structured schedules, and challenges associated with studying in less formal, at-home environments. This observation is consistent with other research indicating that remote education can lead to a decline in discipline and productivity, particularly when students are isolated from the traditional classroom setting (Pelikan et al., 2021). The findings suggest that students in medical programs, which demand high levels of engagement and structure, may have been especially vulnerable to these disruptions. Furthermore, the emotional strain of adjusting to this new educational format further exacerbated these challenges.
The emotional impact of remote learning emerged as a significant finding in our study. Many students expressed negative feelings such as sadness, frustration, and anxiety, often connected to uncertainty about the future, loss of social interactions, and the inability to engage in practical, hands-on activities. This is consistent with research indicating that social isolation and the lack of in-person engagement during the pandemic have negatively affected students’ mental health (Son et al., 2020). In medical education, where peer collaboration and mentorship are vital to the learning experience, the absence of these social interactions may have led to feelings of withdrawal and disengagement. Furthermore, Guckian et al. (2021) noted that over 3.81 billion active social media users worldwide contribute to medical education by enhancing professionalism, blended learning, well-being, and mentoring within undergraduate programs. Nevertheless, earlier systematic reviews conducted prior to the recent surge in social media usage revealed a lack of high-quality empirical studies assessing its effectiveness in the context of medical education.
One of the primary weaknesses highlighted in the study was the inadequacy of online education for practical and laboratory-based learning, which is crucial for medical training. Participants consistently pointed out that, although online lectures provided certain advantages—such as easy access and the convenience of re-watching recorded sessions – they could not substitute for the hands-on experience essential in medical fields. Chick et al. (2020) observed that significant technical difficulties disrupted learning for many students, aligning with our findings on the prevalence of technical issues reported by medical students. This important observation emphasizes the limitations of remote education for subjects that require experiential learning, which is difficult to replicate in a virtual setting (Dedeilia et al., 2020). The absence of practical skill development and reduced opportunities for direct interaction with instructors impeded students’ ability to engage with and comprehend the material thoroughly.
A commonly cited challenge during the pandemic was the prevalence of technical issues, such as unreliable internet access and platform failures, which disrupted the learning process. These challenges were not unique to medical students; they have been widely reported across higher education (Pokhrel & Chhetri, 2021). However, these issues were particularly detrimental for medical students because maintaining concentration during complex theoretical and clinical lessons is crucial. These disruptions likely contributed to feelings of frustration and disengagement among students.
Chick et al. (2020) introduced a flipped classroom strategy for specific conferences. In this well-supported teaching method, learners are provided with didactic materials through prerecorded video lectures, which they can view at their convenience prior to the conference. The authors transitioned weekday academic conferences to a teleconference format using GoToMeeting (LogMeIn Inc.), enabling trainees and staff to participate via live video. This approach allows lecturers to see participants, pose questions, and foster an interactive experience akin to in-person meetings. While most users log in from computers, the platform is also accessible on smartphones and tablets, enhancing engagement from any location. Comparable tools like Zoom, WebEx, and Skype offer similar functionalities. Furthermore, conferences (except those containing protected information) are recorded and stored in the cloud for residents to access later.
Interestingly, despite the various challenges encountered, many participants reported an increase in their GPA during the remote education period. This suggests that the flexibility of online learning—such as the ability to study at one’s own pace and eliminate time-consuming commutes—may have enabled students to manage their time more effectively. However, several participants expressed skepticism about the validity of these GPA improvements, arguing that higher grades do not necessarily indicate enhanced learning or a deeper understanding of the subject matter. This raises concerns regarding the long-term implications of remote learning for students’ readiness for clinical practice and examinations.
Although most participants encountered challenges, a smaller group exhibited resilience and adaptability, demonstrating their success in adjusting to the remote education model. This finding underscores the varying degrees of student adaptability, which may be influenced by individual learning styles, access to resources, and the level of institutional support. Future research could investigate strategies to assist students who face difficulties during such transitions, particularly in fields that demand intensive, hands-on training.
The findings emphasize the need for a more structured and interactive approach to online medical education. While theoretical content can be effectively delivered through online platforms, practical learning components should be preserved in face-to-face formats. Furthermore, medical programs should focus on enhancing the interactivity of online courses, ensuring that students have ample opportunities to interact with instructors and peers. Integrating technologies that facilitate simulation-based learning should also be prioritized whenever possible.
In conclusion, the shift to remote education during the COVID-19 pandemic presented both opportunities and challenges for medical students. While many students appreciated the flexibility that online learning offered, the overwhelming majority faced difficulties due to the lack of practical learning experiences, social interaction, and structured routines. These findings indicate that, although online education has its place in medical curricula, it must be thoughtfully balanced with in-person training to support the development of both theoretical knowledge and practical skills. Additionally, addressing technical issues and providing mental health support will be vital for enhancing the remote learning experience in the future.
5. Conclusion and Recommendations
The study highlights the substantial impact that remote education had on students’ academic habits, emotional responses, and overall educational experiences during the COVID-19 pandemic. Several key themes emerged from the research, shedding light on the challenges and occasional benefits of this unprecedented shift in learning methods.
Participants reported significant disruptions to their study routines, with many struggling to maintain focus and motivation in a less structured and more isolated environment. Emotional strain played a crucial role, with feelings of uncertainty, sadness, and frustration particularly pronounced. The findings also indicated that technical issues posed a widespread challenge, complicating the transition to online learning. Nevertheless, some students adapted by embracing digital engagement and using recorded lectures.
Regarding emotional responses, the shift to remote education increased negative emotions, such as social isolation and anxiety about future academic and career prospects. However, some students exhibited resilience, discovering ways to cope with these challenges, especially by taking advantage of online education’s flexibility.
The analysis of distance medical education underscored that the online format adversely affected specific disciplines, particularly those that necessitate hands-on practice. While some students valued the convenience of accessing recorded lectures, the lack of practical learning and interaction significantly detracted from their educational experience. Notably, the study revealed that online education positively impacted many students’ GPAs, likely due to the greater flexibility in managing their time and accessing resources. However, some students expressed that the increase in grades appeared somewhat artificial, as it did not necessarily correlate with improved learning outcomes.
Overall, the findings suggest that remote education provided benefits such as flexibility and enhanced GPAs for some students, but the challenges faced were more pronounced. The emotional and academic difficulties encountered during the pandemic—including disrupted routines, technical challenges, and insufficient practical learning opportunities—highlight the urgent need for structured support and more interactive, hands-on elements in future online education. These findings emphasize the importance of addressing students’ mental well-being and developing adaptable, student-centered approaches to remote learning.
One promising direction is the development and implementation of hybrid learning models that combine the flexibility of online learning with the essential hands-on experiences of face-to-face education. This is particularly important in medical education, where practical and laboratory-based learning cannot be fully replicated online. Future research could investigate the optimal balance between virtual and in-person education, especially for training in clinical skills.
Additionally, the emotional strain many students have experienced during remote education highlights the need for improved mental health support. Future initiatives should focus on integrating mental health resources into online education platforms. This could include counselling, peer support groups, and stress management workshops. Research could also explore the specific mental health needs of medical students and develop targeted interventions to address these challenges in both online and in-person learning environments.
Given students’ diverse experiences and capacity for adaptability, future studies should consider exploring personalized teaching strategies that recognize and address individual learning styles and needs. The potential of adaptive learning technologies, which can respond to medical student performance and deliver tailored content or support, warrants further examination to address students’ varying levels of engagement and success effectively. Additionally, it would be beneficial for future research to investigate the long-term effects of the COVID-19 remote education experience on medical students’ academic performance, career development, and mental health. Such studies could provide valuable insights into how healthy students transition back to in-person education and whether the skills or habits cultivated during distance learning continue to influence their medical careers.
Bibliography
Ahmady, S., Kallestrup, P., Sadoughi, M. M., Katibeh, M., Kalantarion, M., & Amini, M. (2021). Distance learning strategies in medical education during COVID-19: A systematic review. Journal of Education and Health Promotion, pp. 10, 421.
Akan, H., Şahin, B., Usta, M., Özay, Ö., Yüzüak, H., & Oğuz, U. (2021). Pandemi döneminde tıp eğitimini sürdürmek: Giresun Üniversitesi Tıp Fakültesi deneyimi. Tıp Eğitimi Dünyası, 20(60-1), 54-58.
Asma, B., & Tezci, I. H. (2023). Academician perspective on the implementation of distance education in universities during the Covid-19 pandemic. Journal of Qualitative Research in Education, 34, 86–113. https://doi.org/10.14689/enad.34.912
Başer, D. A., Ağadayı, E., & Karagöz, N. (2020). Bir tıp fakültesi öğrencilerinin pandemide uzaktan eğitim ile ilgili davranışları ve sorunları pandemi sürecinde tıp eğitimi. The Journal of Turkish Family Physician, 11(4), 149-158.
Chick, R. C., Clifton, G. T., Peace, K. M., Propper, B. W., Hale, D. F., Alseidi, A. A., & Vreeland, T. J. (2020). Using technology to maintain the education of residents during the COVID-19 pandemic. Journal of Surgical Education, 77(4), 729–732. https://doi.org/10.1016/j.jsurg.2020.03.018
Clark, J. T. (2020). Distance education. In Clinical engineering handbook (2nd ed., pp. 410–415). Elsevier. https://doi.org/10.1016/B978-0-12-813467-2.00063-8
Coman, C., Tiru, L. G., Schmitz, L. M., Stanciu, C., & Bularca, M. C. (2020). Online teaching and learning in higher education during the coronavirus pandemic: Students’ perspective. MDPI Journal, 12(24), 1–24.
Daroedono, E., Siagian, F. E., Alfarabi, M., Cing, J. M., Arodes, E. S., Sirait, R. H., … & Hutabarat, R. S. O. (2020). The impact of COVID-19 on medical education: Our students’ perception on the practice of long-distance learning. International Journal of Community Medicine and Public Health, 7(7), 2790–2796.
Dedeilia, A., Sotiropoulos, M. G., Hanrahan, J. G., Janga, D., Dedeilias, P., & Sideris, M. (2020). A systematic review of medical and surgical education challenges and innovations in the COVID-19 era. In Vivo, 34(3 Suppl), 1603–1611.
Dron, J. (2021). Technology, teaching, and the many distances of distance learning. Journal of Open, Flexible and Distance Learning, 25(1), 1–20. Retrieved from https://jondron.ca
Gunawardena, C. N., & McIsaac, M. S. (2013). Distance education. In Handbook of research on educational communications and technology (pp. 361–401). Routledge.
Guckian, J., Utukuri, M., Asif, A., Burton, O., Adeyoju, J., Oumeziane, A., Chu, T., & Rees, E. L. (2021). Social media in undergraduate medical education: A systematic review. Medical Education, 55(11), 1227–1241. https://doi.org/10.1111/medu.14567
Hughes, B. A., Stallard, J., & West, C. C. (2020). The use of WhatsApp® as a way to deliver plastic surgery teaching during the COVID-19 pandemic. Journal of Plastic, Reconstructive & Aesthetic Surgery, p. 73, e1–e2.
Kentnor, H. E. (2015). Distance education and the evolution of online learning in the United States. Curriculum & Teaching Dialogue, 17.
Moore, M. G., & Kearsley, G. (2012). Distance education: A systems view of online learning (3rd ed.). Wadsworth.
Panahi, P., & Borna, F. (2014). Distance learning: Challenges, new solution. In 2014 37th International Convention on Information and Communication Technology, Electronics and Microelectronics (MIPRO) (pp. 653–656). https://doi.org/10.1109/MIPRO.2014.6859648
Patton, M. Q. (2014). Qualitative research & evaluation methods: Integrating theory and practice. Sage Publications.
Pelikan, E. R., Lüftenegger, M., Holzer, J., Korlat, S., Spiel, C., & Schober, B. (2021). Learning during COVID-19: The role of self-regulated learning, motivation, and academic stress in remote higher education. Frontiers in Psychology, 12, 687.
Pokhrel, S., & Chhetri, R. (2021). A literature review on the impact of COVID-19 pandemic on teaching and learning. Higher Education for the Future, 8(1), 133–141.
Schneider, S. L., & Council, M. L. (2021). Distance learning in the era of COVID-19. Archives of Dermatological Research, 313(5), 389–390. https://doi.org/10.1007/s00403-020-02088-9
Siddiqui, U. D., & Aslanian, H. R. (2020). The new virtual reality: Advanced endoscopy education in the COVID-19 era. Digestive Diseases and Sciences, 65(7), 1888–1891. https://doi.org/10.1007/s10620-020-06386-0
Sindiani, A. M., Obeidat, N., Alshdaifat, E., Elsalem, L., Alwani, M. M., Rawashdeh, H., … & Tawalbeh, L. I. (2020). Distance education during the COVID-19 outbreak: A cross-sectional study among medical students in North of Jordan. Annals of Medicine and Surgery, 59, 186–194.
Son, C., Hegde, S., Smith, A., Wang, X., & Sasangohar, F. (2020). Effects of COVID-19 on college students’ mental health in the United States: Interview survey study. Journal of Medical Internet Research, 22(9), e21279.
Totaro, M. W., Tanner, J. R., Noser, T. C., Fitzgerald, J. F., & Birch, R. (2005). Faculty perceptions of distance education courses: A survey. Journal of College Teaching & Learning, 2(7), 13–20.
Tran, B. (2016). Educational experiences with traditional, online, and hybrid learning environments. Journal of Education & Social Policy, 3(3), 60–65.
UNESCO. (2020). COVID-19 educational disruption and response. United Nations Educational, Scientific and Cultural Organization. https://en.unesco.org/themes/education-emergencies/coronavirus-school-closures
WHO. (2021). Coronavirus disease (COVID-19) outbreak situation. World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus
Yıldırım, A. & Şimşek, H. (2018). Qualitative research methods in the social sciences. Seçkin Publishing: Ankara.
YÖK. (2020). Higher Education in Turkey: Medical Education and Training. Council of Higher Education.
Zhong, R. (2020, March 17). The coronavirus exposes education’s digital divide. The New York Times. https://www.nytimes.com/2020/03/17/technology/china-schools-coronavirus.html
Acknowledgements
We utilized Grammarly (2024) to support language editing throughout the manuscript. For reference: Grammarly (Nov 25 version) [Large language model]. (2024). Retrieved from https://app.grammarly.com
Funding Information: This study received no specific grant from public, commercial, or not-for-profit funding agencies.
Competing Interests: The authors have no competing interests to declare.
Author Contributions: Miray Dogan: Conceptualization, Handan Ak. & Hakan Aydin Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – review & editing. Arda Celik: Conceptualization, Formal Analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. All authors have read and agreed to the published version of the manuscript.
Ethics and consent: This study was approved by the Ege University Medical Research Ethics Committee (Approval No: 23-5.1T/32, Date: 30.05.2023-E.1288956). The research was conducted at Ege University, Faculty of Medicine, Department of Medical Biochemistry in Turkey.
____________________
Authors:
Miray Dogan
mraydogan@ymail.com – corresponding author
Department of Educational Sciences, Faculty of Education, Çanakkale 18 Mart University, Çanakkale, Türkiye
![]() https://orcid.org/0000-0002-6734-8947
https://orcid.org/0000-0002-6734-8947
Arda Celik
Department of Electrical, Computer, and Software Engineering, Faculty of Engineering and Applied Science, Ontario Tech University, Ontario, Canada
![]() https://orcid.org/0009-0000-7339-0183
https://orcid.org/0009-0000-7339-0183
Handan Ak
Department of Medical Biochemistry, Faculty of Medicine, Ege University, İzmir, Türkiye
![]() https://orcid.org/0000-0002-3261-0036
https://orcid.org/0000-0002-3261-0036
Hikmet Hakan Aydın
Department of Medical Biochemistry, Faculty of Medicine, Ege University, İzmir, Türkiye
![]() https://orcid.org/0000-0002-4387-6745
https://orcid.org/0000-0002-4387-6745
Received: 10.01.2025. Accepted: 18.02.2025
© Miray Dogan, Arda Celik, Handan Ak, Hikmet Hakan Aydın, 2025. This open access article is distributed under the terms of the Creative Commons Attribution Licence CC BY, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited:
Citation:
Dogan, M., Celik, A., Ak, H., & Aydin, H. H. (2025). The Perspective of Medical School Students on Distance Education. Journal of Digital Pedagogy, 4(1) 36-48. Bucharest: Institute for Education. https://doi.org/10.61071/JDP.2524
